Facilities
Health Sciences Laboratory Spaces
The new lab space within ODUs in the newly constructed Ellmer College of Health Sciences building has four dedicated laboratory spaces. These contain our new virtual reality treadmill system, a complete motion capture lab, and transcranial magnetic stimulation equipment. Also within the building is the Faschini Wallach Center for Restorative Therapies, a state-of-the-art 11,000-square-foot rehabilitation facility that allows easy access to clinical populations and researchers. Additional KR-affiliated lab spaces across campus include the Human Performance Laboratory, Neuromechanics Laboratory, and Integrative Cardiometabolic Laboratory.
Research Topics
Athletes with lower extremity joint injuries commonly return to sport before all structure and functional impairments are resolved. Additionally, athletes commonly experience recurrent injury and chronic joint instability, particularly following an ankle sprain. Thus, within our School, we aim to identify factors contributing to recurrent injury and chronic instability. Community-based studies involving high school and collegiate athletes and clinical athletic trainers examine the predictive value of common clinical evaluation and care techniques used by athletic trainers. Information from this area can improve long-term outcomes for injured athletes and enhance the efficiency of care provided by athletic trainers.
Selected Publications:
- McCann RS, Squillantini R, Suttmiller AMB, Chung S. Patient-Reported Outcome Scores of Athletes with Time-Loss and Non-Time-Loss Ankle Sprains. International Journal of Athletic Therapy & Training. In Press.
- McCann RS, Ohrnberger E, Kosik KB, Gribble PA. Prediction of Recurrent Lateral Ankle Sprain and Ankle Pain Using Applied Care Strategies and Patient-Reported Outcomes. Journal of Athletic Training. In Press.
- McCann RS, Welch Bacon CE, Suttmiller AMB, Gribble PA, Cavallario JM. Influences of Athletic Trainers' Return-to-Activity Assessments for Patients with an Ankle Sprain. Journal of Athletic Training. 2024, 59(2):201-211.
- McCann RS, Welch Bacon CE, Suttmiller AMB, Gribble PA, Cavallario JM. Assessments Used by Athletic Trainers to Decide Return-to-Activity Readiness in Patients with an Ankle Sprain. Journal of Athletic Training. 2024, 59(2):182-200.
- McCann RS, Suttmiller AMB, Gribble PA, Cavallario JM. Athletic Trainers’ Methods for Determining Return to Activity for Patients with an Ankle Sprain Part I: Types of Measures Used. International Journal of Athletic Therapy & Training. 2022, 27(2):85-90.
Research on Early Intervention and Neurodevelopmental Outcomes
Our research focuses on early detection and intervention to improve developmental outcomes in children with neurodevelopmental delays, including those born preterm and those diagnosed with autism. Key areas of investigation include the impact of early interventions in the neonatal intensive care unit (NICU), the feasibility of Electroencephalography (EEG) in typically developing children (4-8 years) to study brain activity during walking and comparing the neural correlates of walking between typically developing children and those with autism spectrum disorder (ASD). Additionally, we explore the effects of adaptive gymnastics on motor development in children with autism, aiming to enhance motor skills and overall development.
Selected Publications:
- Poojari DP, Umakanth S, Maiya GA, Rao BK, Khurana S, Kumaran D S, Attal R, Brien M. Effect of family-centered care interventions on well-being of caregivers of children with cerebral palsy: a systematic review. F1000Res. 2024 May 29;12:790. doi: 10.12688/f1000research.133314.2. PMID: 38911944; PMCID: PMC11193087.
- Nayaka NN, Shakya S, Gudi N, Khurana S, Gopalakrishnan S, Rao V, Rao BK. Clothing design solutions for children with developmental disabilities: A scoping review protocol MethodsX. 2024;13:102974. doi:10.1016/j.mex.2024.102974
- Inamdar K, Khurana S, Dusing SC. Effect of Contingency Paradigm-Based Interventions on Developmental Outcomes in Young Infants: A Systematic Review. Pediatr Phys Ther. 2022 Apr 1;34(2):146-161.
- Khurana S, Rao BK, Lewis LE, Kumaran SD, Kamath A, Einspieler C, Dusing SC. Neonatal PT Improves Neurobehavior and General Movements in Moderate to Late Preterm Infants Born in India: An RCT. Pediatr Phys Ther. 2021 Oct 1;33(4):208-216. doi: 10.1097/PEP.0000000000000824. PMID: 34618744.
- Khurana S, Evans ME, Kelly CE, Thompson DK, Burnsed JC, Harper AD, Hendricks-Muñoz KD, Shall MS, Stevenson RD, Inamdar K, Vorona G, Dusing SC. Longitudinal Changes in the Sensorimotor Pathways of Very Preterm Infants During the First Year of Life With and Without Intervention: A Pilot Study. Dev Neurorehabil. 2021 Oct;24(7):448-455. doi: 10.1080/17518423.2021.1903602.
- Khurana S, Kane AE, Brown SE, Tarver T, Dusing SC. Effect of neonatal therapy on the motor, cognitive, and behavioral development of infants born preterm: a systematic review. Dev Med Child Neurol. 2020 Jun;62(6):684-692.
Advancing the outcomes related to educational competency development and implementation for students currently enrolled in AT, PT, OT, or RT programs is pivotal for advancement in each respective field. Understanding effective methods to provide continuing education to practicing clinicians is also critical for professional advancement and offers unique challenges for educators. These areas are particularly concerning for developing competency in evidence-based practice in all clinicians and health professions. Specific areas of educational research in our department are related to effective pedagogical and andragogical techniques for healthcare education delivery, the opportunities for students to engage in patient care during the clinical education, understanding the role of preceptors and program faculty in educational outcomes.
Selected Publications:
- Cavallario JM, Campbell TR, Welch Bacon CE. Lecture-based instruction on salary negotiation for professional athletic training students: an educational technique. Athl Train Educ J. 2024; 19(3): 168-172. https://doi.org/10.4085/1947-380X-24-001
- Welch Bacon CE, Cavallario JM, Walker SE, Bay RC, Van Lunen BL. Athletic training students’ use of evidence-based practice professional behaviors during clinical experiences: a report from the AATE Research Network. Intl J Athl Ther Train. 2024; 29(5): 285-290. https://doi.org/10.1123/ijatt.2023-0132
- Claiborne DM, Durgampudi P, Dumadag AC, Hawkins EJ, Laverdure P, Yaroch-Meeker A, Kraj B, Wilson A, Akpinar M. Health profession students’ Interprofessional Socialization and Values towards a college-based virtual interprofessional education activity. Journal of Allied Health. 2023;52(4):243-249.
- Cavallario JM, Van Lunen BL, Walker SE, Bay RC, Welch Bacon CE. The influence of gender in preceptor-student dyads on student performance in clinical education: a report from the AATE Network. J Allied Health. 2023; 52(2):113-119.
- Cavallario JM, Van Lunen BL, Hoch JM, Hoch MC, Manspeaker SA, Pribesh S. Athletic training student core competency implementation during patient encounters. J Athl Train. 2018; 53[3]. https://doi.org/10.4085/1062-6050-53.3.205
Selected Presentations
- Mariano, M. and Mohn-Johnsen, S. The Touchy Subject: Threading Professional Boundaries in Physical Therapy Education and Practice. Education session at ACAPT/APTA Education Leadership Conference (ELC), October 19, Oakland, California.
- Laverdure, P., Leo, A., Richardson, E., & Andelin, L. (2024, October 9). Collaborative processes to optimize fieldwork participation, experiences, and outcomes: A statewide approach. American Occupational Therapy Association 2024 Education Summit.
- Andelin, L. & Lemmon, A. (2024, October 27). Data-driven decision making model (DDDM): A framework for evidence based practice. Virginia Occupational Therapy Association (VOTA) Annual Conference. Lynchburg, VA.
- Hawkins EJ, Cavallario J. Many paths, one journey: How educators incorporate social determinants of health into DPT curricula. Oral platform presentation at: Educational Leadership Conference; October 2024; Oakland, CA.
- Hawkins EJ, Horvath E, Gustin T. Humanism unveiled: Exploring interprofessional healthcare students’ attitudes towards individuals experiencing homelessness. Poster presented at: Educational Leadership Conference; October 2024; Oakland, CA.
The Monarch Balance for Life program is a key component of the Ellmer College of Health Sciences’ commitment to advancing research in healthy aging. Focused on falls prevention, the program bridges research and practice to deliver cutting-edge, evidence-based care in our community. Through partnerships with independent and assisted living facilities, local health departments, municipal EMS, parks and recreation programs, and for-profit insurance companies, we conduct innovative studies that inform real-world applications. These collaborations enable us to address fall risk from multiple perspectives, translating research findings into actionable strategies that improve mobility, enhance safety, and promote quality of life for aging individuals in our community.
Selected Publications:
- Samulski B, Langerhans K, and Moxey, J. (2024). North American Society for the Psychology of Sport and Physical Activity Conference Abstracts. The correlation of physiological profile assessment, fall-risk index, and gait parameters of community-dwelling older adults. Journal of Sport and Exercise Psychology, 46(S1), S1-104. https://doi.org/10.1123/jsep.2024-0136
- Moxey, J, Langerhans K, Prupetkaew, P and Samulski B. (2024). North American Society for the Psychology of Sport and Physical Activity Conference Abstracts. Performance on cognitive assessments is related to falls risk in community-dwelling older adults. Journal of Sport and Exercise Psychology, 46(S1), S1-104.
- Samulski B, Langerhans K, Moxey J, and Morrison S. (2024). CSM 2024 Platform Abstracts. The Influence of Cognitive Status and Fear of Falling on Falls Risk and Reported Falls. Journal of Geriatric Physical Therapy, 47(1), E19-E47, January/March 2024.
Our research on motor control examines how the brain regulates movement across the lifespan, helping us distinguish typical patterns of development and aging from those indicative of pathology or functional impairment. Very little is known about how older bodies move, and improving our understanding is essential to helping people stay healthy and active for a greater portion of their lives. One study area investigates the effect of gum chewing on gait patterns and its potential use as an external cue to improve gait in adults diagnosed with Parkinson’s disease. By uncovering insights into how motor control changes with age, we aim to develop innovative, evidence-based strategies to support functional mobility and enhance quality of life across diverse populations.
Selected Publications:
- Prebor, J, Samulski, B, Armitano-Lago, C, & Morrison, S. (2023). Patterns of Movement Performance and Consistency From Childhood to Old Age. Motor Control. 27(2), 258-274.
- Prebor, J., Samulski, B., Armitano-Lago, C., & Morrison, S. (2021). Chewing Entrains Cyclical Actions but Interferes With Discrete Actions in Children. Journal of Motor Behavior, 1-9.
- Samulski B, Prebor J, Armitano C, Morrison S. (2020). Age-related changes in neuromotor function when performing a concurrent motor task. Experimental Brain Research, 1-10.
- Samulski B, Prebor J, Armitano C, Morrison S. (2019) Coupling of motor oscillators- What really happens when you chew gum and walk? Neuroscience Letters, 698:90-96.
- Samulski B, Prebor J, Armitano C, Morrison S. (2018). Chewing rates resistant to age-related slowing and may be novel rehabilitation technique for rhythmic cuing. Archives of Physical Medicine and Rehabilitation, 99. e99.
Childhood
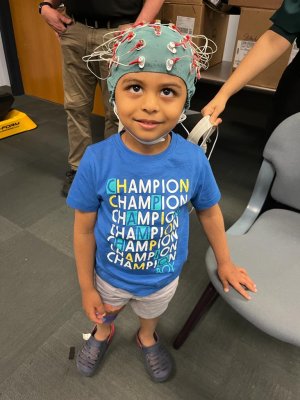
Early childhood is a critical period of learning and development for young children. We are investigating how children learn and develop skills in emotion regulation, emergent literacy (explicitly writing), and play. Our research involves interprofessional collaboration with researchers in professions such as Speech/Language Pathology, Special Education, and Physical Therapy. (image: childhood, Peds emg)
People with Intellectual & Developmental Disabilities (IDD)
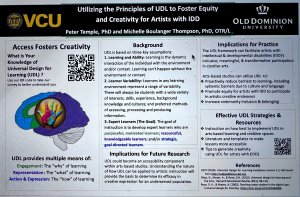
We investigate how creativity, UDL, and belonging enhance equity and inclusion for people with intellectual and developmental disabilities (IDD). Our research involves interprofessional collaboration with researchers in professions such as Human Development and Medical Anthropology. (Image: occupational IDD)
Selected Publications:
- Thompson MB, Xu Y, Chen CC, Rudasill K. Empowering and Educating Parents to Implement a Home Intervention: Effects on Preschool Children's Engagement in Hands-on Constructive Play. Behav Sci (Basel). 2024 Mar 19;14(3):247. doi: 10.3390/bs14030247. PMID: 38540550; PMCID: PMC10968168.
Emergency action plans (EAPs) and policies & procedures are critical tools in preventing sudden death in sport, where the leading causes include sudden cardiac arrest, exertional heat stroke, exertional sickling, traumatic brain injury, and cervical spine trauma. Athletic trainers are uniquely positioned as frontline healthcare providers to both develop and implement these plans, ensuring rapid recognition and coordinated response when emergencies occur. Research has highlighted numerous facilitators, barriers, and contextual factors that influence the adoption of EAPs ranging from organizational support and community partner buy-in to resource limitations and competing priorities. While this body of evidence has advanced our understanding of why EAPs are or are not effectively implemented, there remains a pressing need to design and test tailored strategies that improve compliance with best-practice standards across all levels of sport. By equipping athletic trainers and institutions with actionable, context-specific tools, we can close the gap between policy and practice and ultimately reduce preventable deaths in athletes.
Select Citations:
- Scarneo-Miller SE, Hosokawa Y, Drezner JA, Hirschhorn RM, Conway DP, Elkins GA, Hopper MN, Strapp EJ. National Athletic Trainers’ Association Position Statement: Emergency Action Plan Development and Implementation in Sport. J Athl Train. 2024;59(6):570-583.
- Scarneo-Miller SE, Stearns RL, Eason CM, Pike Lacy AM, Lopez RM, Winkelmann ZK, Hirschhorn RM, Yeargin SW. Emergency Action Plan Adoption Across Athletic Training Practice Settings. J Athl Train. Published online 2025. doi:10.4085/1062-6050-0255.25
- Scarneo-Miller SE, DiStefano LJ, Register-Mihalik JK, Stearns RL, Denegar CR, Casa DJ. Emergency Action Plans in Secondary Schools: Barriers, Facilitators, and Social Determinants Affecting Implementation. J Athl Train. 2020;55(1):80-87.
- Scarneo-Miller SE, DiStefano LJ, Stearns RL, Register-Mihalik JK, Denegar CR, Casa DJ. Emergency Action Planning in Secondary-School Athletics: A Comprehensive Evaluation of Current Adoption of Best Practice Standards. J Athl Train. 2019;54(1):99-105.
Several joint injuries are associated with residual deficits in both sensory and motor aspects of function. Further defining sensorimotor alterations following injury may lead to novel intervention strategies to enhance short-term recovery, reduce the long-term implications, and prevent many injuries. The research conducted in our School is primarily focused on sensorimotor issues related to ankle and knee injuries. Specifically, recent studies have focused on measures of impaired neuromuscular control (strength, muscle activation, functional movement patterns, etc.) related to chronic ankle instability and anterior cruciate ligament injuries. Furthermore, neural excitability tests identify changes to the central nervous system that contribute to neuromuscular impairments. In addition to defining new areas of sensorimotor compromise, research is also being conducted to identify novel strategies to address these types of impairments and activity limitations in individuals with an injury history or those at risk.
Selected Publications:
- Suttmiller AMB, Chung S, Gruskiewicz V, Johnson K, Foreman N, Reyes M, McCann RS. Comparing the Effects of Progressive Balance and Hip-Strengthening Rehabilitation in Individuals with Chronic Ankle Instability. Journal of Sport Rehabilitation. In Press.
- Reyes M, Suttmiller AMB, Chung S, Gruskiewicz V, Johnson K, Foreman N, McCann RS. Cross-Education Effects of Balance Training in Individuals with Chronic Ankle Instability. Journal of Bodywork & Movement Therapies. 2024, 40:1263-1268.
- Chung S, Rodriguez A, Alijanpour E, McCann RS. Effects of a Single Balance Training Session on Neural Excitability in Individuals with Chronic Ankle Instability. Journal of Sport Rehabilitation. 2023, 32(8):847-854.
- McCann RS, Johnson K, Suttmiller AMB. Lumbopelvic stability and trunk muscle contractility of individuals with chronic ankle instability. International Journal of Sports Physical Therapy. 2021, 16(3):741-748.
- Thompson T, Suttmiller AMB, Ringle B, McCann RS. Corticomotor Excitability of the Gluteus Maximus in Individuals with Chronic Ankle Instability: A Pilot Study. Translational Sports Medicine. 2021, 4(1):65-71.
Sports-related concussions represent a significant risk when participating in athletic activities. Following concussion, most symptoms typically last for approximately 7 to 10 days. However, there are also long-term consequences of repeated head contact, which include depression, central nervous system impairment, and mild cognitive impairment. Even after recovery, the effects of head trauma can persist, as concussed athletes are at increased risk for lower extremity injury when they return to play. Identifying those who have sustained a concussion remains a primarily subjective process. Our research attempts to identify salivary biomarkers, balance, and coordination deficits that offer diagnostic utility for concussions.
Selected Publications:
- Campbell TR, Reilly N, Zamponi M, et al. Salivary microRNA as a prospective tool for concussion diagnosis and management: A scoping review. Brain Injury. Published online March 3, 2023:1-8. doi:10.1080/02699052.2023.2184867
- Schussler E, Jagacinski R, Buford J, Chaudhari A, Onate J. Effect of Video Feedback on Tackling Performance in Youth Football Athletes. Journal of Athletic Training. 2024; 1:59(3):281-288.
- Ramirez V, Schussler E, Martinez JC, McCann R. Lower extremity injury after concussion: A systematic review. The Effect of Concussion History on Lower Extremity Injury Risk in College Athletes: A Systematic Review and Meta-Analysis. International Journal of Sports Physical Therapy. 2022;17(5):753-765.
- Patejak S, Forrest J, Harting E, Sisk M, Schussler E. A Systematic Review of Center of Mass as a Measure of Dynamic Postural Control Following Concussion. International Journal of Sports Physical Therapy. International Journal of Sports Physical Therapy. 2021. 16(5), 1222-1234.
- Schussler E, Jagacinski RJ, White SE, Chaudhari AM, Buford JA, Onate JA. The Effect of Tackling Training on Head Accelerations in Youth American Football. International Journal of Sports Physical Therapy. 2018; 13(2).
- Reilly N, Prebor J, Moxey J, Schussler E. Chronic impairments of static postural stability associated with history of concussion. Experimental Brain Research. 2020. 238, 2783-2793.